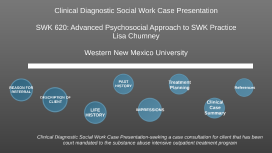
Clinical Diagnostic Social Work Case Presentation
Transcript: Clinical Diagnostic Social Work Case Presentation Date 1 Ebony L. Welch Western New Mexico University Reason for Referral and Presenting Problem Presenting Problem Client: Cindy Woods Cindy presents with a history of suicidal and homicidal ideations, self-injurious behaviors, auditory hallucinations, delusions, disorganized thoughts, and substance use disorder. Per her medical records, she stated that "there are worms under her skin and people in the television who want to watch me die." She also states that voices are telling her to kill herself and others. Cindy was jailed and taken to the hospitals, emergency department, then transferred to an in-patient psychiatric facility for 30 days. Cindy was referred for individual psychotherapy, following the 30 days in-patient psychiatric hospitalization. Description of Client Client's History 54 year old Caucasian female 20+ years of Chronic Homelessness 2 Children (33y/o Jane & 35y/o John) Estranged from both children/ No support system Divorced from ex-husband Currently on Social Security Disability (SSDI) $800/m Methamphetamine and Cocaine dependency Disorganized thoughts/speech Cognitive functioning: low during psychosis Moderate cognitive functioning w/out psychosis Appearance: Appropriate. Although clothes are ill fitted Mood: Anxious Brief Pertinent Life History Brief Life History Cindy's family has a history of Severe mental illness (Schizophrenia) Childhood neglect and maltreatment Alcohol and substance abuse Cindy reports being homeless for more than 20 years after her home caught fire. She has stayed in temporary shelters and on the street. The client also reports intimate partner violence by her ex-husband for the extent of their marriage. The client reports extensive suicidal ideations and attempts due to hopelessness, isolation, and lack of resources. The client reports extensive legal history, with several arrest. Past Psychiatric History Past Psychiatric History The client has an extensive history of in-patient psychiatric hospitalization. She reports three in-patient psychiatric hospitalizations lasting 30 days or more, with the most recent admissions being May 2019 and early Jan 2020. In Jan, the client presented with self-injurious behaviors, auditory hallucinations, delusions, disorganized thoughts/speech. Per her medical records, Cindy stated that she harms herself "when it is necessary." On the Jan occasion, per her chart, when asked about her religious/spiritual beliefs she stated "I like to burn bibles." She also stated that "the worms under her skin multiply" when she takes her medication. Upon discharge in Feb 2020, the client followed up with Mental Health Mental Retardation (MHMR) Services, Risk Assessment Care Team (RACT), and MHMR respite for housing. Upon discharge she expressed that she wanted to continue to get well, so that she could get her social security card, state ID, and birth certificate to get an apartment. She also expressed getting healthy to reconnect with her two children. Past Medical History Chronic Obstructive Pulmonary Disease (COPD) Hypothyroidism Noncompliance with medication Clinical Impression of Concerns and Strengths Clinical Impression Axis I: 95.70 (F25.0) Schizoaffective Disorder, Bipolar Type; 304.40 (F15.20) Amphetamine-Type substance, Severe 304.20 (F15.20) Stimulant Use Disorder, Severe: Cocaine Axis II: None Axis III: COPD & Hypothyrodism Axis IV: Chronic homelessness, economic problems, no social support Axis V: Will assess The client's dual diagnosis of substance abuse and psychotic symptoms have gravely contributed to chronic homelessness, poor social support, and impairment in social skills. Strengths: Independent living Sense of humor Willingness to participate with treatment Clinical Impressions of Concerns and Strengths Clinical Impression Cont. Mental health disorders that can be ruled out Schizoaffective disorder depressive type Schizophrenia Delusional disorder The client best meets the criteria for schizoaffective disorder bipolar type rather than the other disorders. Further, Cindy may have a genetic predisposition of psychotic mental illnesses from her father. According to the American Psychiatric Association (2013) individuals who are most at risk for schizoaffective disorders are first degree relatives of those who have schizophrenia, schizoaffective disorders, and bipolar. Treatment Planning Treatment Intervention Approach: Cognitive Behavioral Therapy (CBT) Referrals MHMR Psychiatrist Substance Abuse Treatment program Narcotics Anonymous Workforce solutions (for life skills) Support Group for Severe mental illnesses Treatment Plan Cont. Treatment Plan Cont. Empirical evidence has linked Substance Use with psychotic disorders, specifically those on the schizophrenia spectrum (Nesvag et al., 2015). It is believed that mental health disorders such as schizoaffective have an influential affects on substance usage. Also, combination treatments such as antipsychotic, mood stabilizers, and